Antibiotic resistance has emerged as one of the most significant public health challenges of our time. The ability of bacteria to evolve and resist the effects of antibiotics threatens to undermine decades of medical progress. As a result, infections that were once easily treatable are becoming harder to manage, leading to longer hospital stays, higher medical costs, and increased mortality rates. This article explores the causes, consequences, and potential solutions to the growing threat of antibiotic resistance.
What is Antibiotic Resistance?
Antibiotic resistance occurs when bacteria change in a way that reduces or eliminates the effectiveness of drugs designed to treat infections. These bacteria, often referred to as “superbugs,” can survive and continue to multiply even in the presence of antibiotics. As a result, standard treatments become ineffective, and infections become much more difficult to treat.
Antibiotic resistance is a natural process, but the overuse and misuse of antibiotics in human medicine, agriculture, and animal farming have accelerated the development of resistant bacteria.
Causes of Antibiotic Resistance
The development of antibiotic resistance is driven by several factors, both medical and societal.
1. Overuse of Antibiotics in Human Medicine
One of the leading causes of antibiotic resistance is the overuse and misuse of antibiotics in human healthcare. Many patients request antibiotics for viral infections like the common cold or the flu, which do not respond to antibiotics. Additionally, improper use, such as not completing the full course of prescribed antibiotics, can allow bacteria to survive and develop resistance.
2. Use of Antibiotics in Agriculture and Animal Farming
Antibiotics are frequently used in agriculture and animal farming to promote growth and prevent disease in healthy animals. This widespread use of antibiotics in food production contributes to the emergence of resistant bacteria, which can then spread to humans through the consumption of contaminated meat or direct contact with animals.
3. Inadequate Infection Control in Healthcare Settings
Hospitals and healthcare settings are prime environments for the spread of antibiotic-resistant bacteria. Inadequate infection control measures, such as improper sanitation, lack of hand hygiene, and improper use of antibiotics, can contribute to the transmission of resistant bacteria among patients, healthcare workers, and visitors.
4. Global Travel and Trade
The movement of people, animals, and goods across borders can facilitate the spread of antibiotic-resistant bacteria. Resistant strains can travel with individuals or be carried in food products, leading to the global spread of resistance and complicating efforts to contain infections.
Consequences of Antibiotic Resistance
Antibiotic resistance has wide-reaching implications, both for individuals and society as a whole.
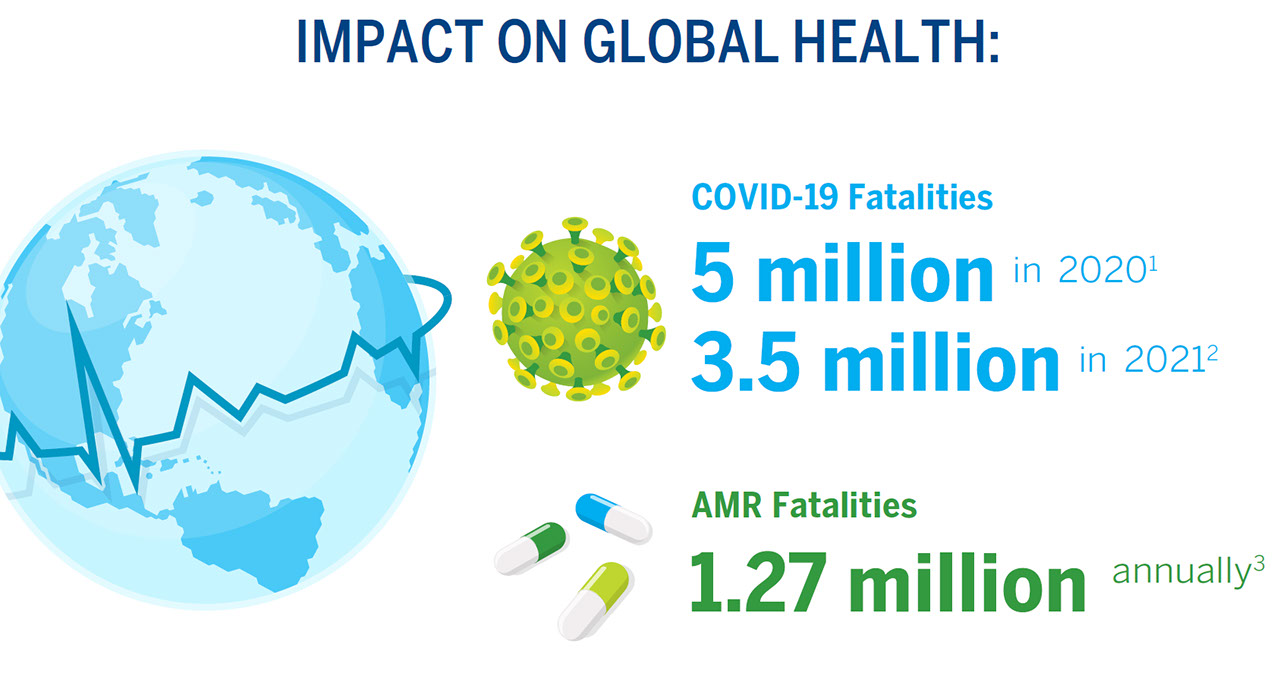
1. Increased Mortality Rates
As antibiotics become less effective, infections that were once easily treatable can become life-threatening. Common surgeries and procedures, such as organ transplants, chemotherapy, and C-sections, rely on the use of antibiotics to prevent infection. Without effective antibiotics, these procedures become riskier, and mortality rates from infections rise.
2. Longer Hospital Stays and Higher Healthcare Costs
Patients with antibiotic-resistant infections require more complex and prolonged treatments. This leads to longer hospital stays, the need for more expensive drugs, and increased healthcare costs. The financial burden of antibiotic resistance extends beyond individual patients, placing strain on healthcare systems worldwide.
3. Limited Treatment Options
As bacteria become resistant to more antibiotics, the treatment options available to healthcare providers diminish. In some cases, infections that were once easily treatable with first-line antibiotics may require the use of older, more toxic drugs, which may have more side effects and be less effective.
4. Threat to Medical Advancements
Antibiotic resistance threatens the progress made in modern medicine. Life-saving treatments, such as organ transplants, cancer chemotherapy, and surgeries, rely on antibiotics to prevent infections. Without effective antibiotics, the safety of these procedures is compromised, potentially reversing decades of medical advancements.
Addressing Antibiotic Resistance
Fighting antibiotic resistance requires a coordinated, multi-faceted approach involving healthcare professionals, governments, pharmaceutical companies, and the general public. Some of the key strategies include:
1. Improving Antibiotic Stewardship
Antibiotic stewardship refers to the responsible use of antibiotics to ensure they are prescribed only when necessary and appropriate. Healthcare providers must prioritize accurate diagnoses, avoid unnecessary prescriptions, and educate patients on the proper use of antibiotics. It is essential to complete the full course of antibiotics to prevent resistance from developing.
2. Increased Surveillance and Monitoring
Tracking the spread of antibiotic-resistant bacteria is critical to controlling its growth. Enhanced surveillance systems can help identify emerging resistant strains and monitor trends in antibiotic resistance. This data can inform public health policies and interventions to prevent the spread of superbugs.
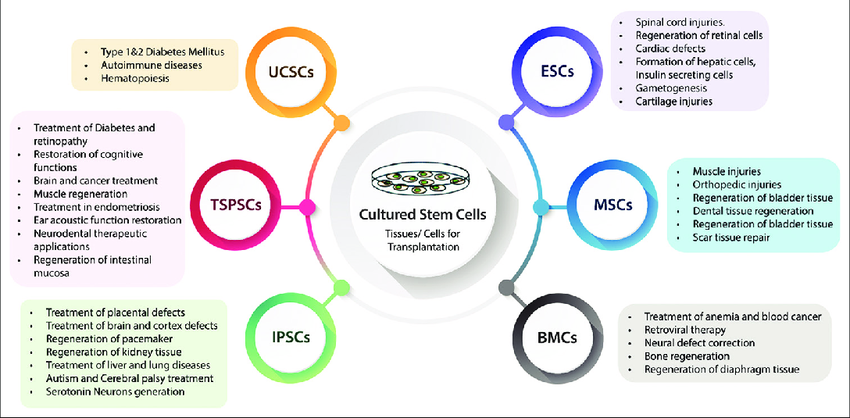
3. Investing in New Antibiotics and Alternatives
Pharmaceutical companies and research institutions must focus on developing new antibiotics and alternative treatments to combat resistant infections. The development of vaccines, bacteriophage therapy, and other innovative therapies could offer new ways to fight infections and reduce the reliance on antibiotics.
4. Improving Infection Control Measures
Healthcare facilities must adopt strict infection control practices to prevent the spread of antibiotic-resistant bacteria. This includes promoting hand hygiene, proper sanitation, isolation of infected patients, and the use of personal protective equipment. Training healthcare workers in infection prevention is essential to minimize the risk of resistance.
5. Public Awareness Campaigns
Educating the public about the dangers of antibiotic misuse is crucial in the fight against resistance. Public awareness campaigns can encourage people to take antibiotics only when prescribed, complete the full course of treatment, and practice good hygiene to prevent the spread of infections. It’s also important to inform people about the risks of using antibiotics in agriculture and the environment.
6. Regulating Antibiotic Use in Agriculture
Reducing the use of antibiotics in livestock farming is essential for limiting the development of resistance. Many countries have implemented or are considering stricter regulations on the use of antibiotics in food production. These measures include restricting the use of antibiotics for growth promotion and ensuring antibiotics are only used to treat sick animals.
The Role of Global Collaboration
Antibiotic resistance is a global issue that requires cooperation among countries, organizations, and sectors. International collaboration is vital in sharing data, coordinating research efforts, and establishing global policies to combat antibiotic resistance. The World Health Organization (WHO) has called for a “One Health” approach, recognizing the interconnectedness of human, animal, and environmental health in the fight against antibiotic resistance.
By working together, countries can implement global surveillance systems, share best practices for antibiotic stewardship, and coordinate efforts to develop new treatments and prevent the spread of resistance.
Conclusion
Antibiotic resistance is a growing global threat that has the potential to reverse decades of medical progress and lead to higher mortality rates, longer hospital stays, and greater healthcare costs. The overuse and misuse of antibiotics in human medicine, agriculture, and animal farming have accelerated the development of resistant bacteria, creating urgent challenges for healthcare systems worldwide.
To address this issue, a collaborative approach is necessary, focusing on improving antibiotic stewardship, increasing research into new treatments, and educating the public on responsible antibiotic use. By taking immediate action, we can slow the spread of antibiotic resistance and preserve the effectiveness of antibiotics for future generations. The fight against antibiotic resistance is not only a medical challenge but also a global responsibility that requires the collective efforts of individuals, healthcare providers, governments, and organizations worldwide.